What is the microbiome, and how can we use it to treat disease?
Once relegated to the realm of alternative medicine, the microbiome – the presence and actions of trillions of microorganisms dwelling on and in our body – is increasingly being revealed as a potent driver of myriad diseases.
Now, researchers are looking for ways to harness these populations of microscopic hangers-on as therapies for as-yet incurable conditions.
Our microbiome’s demographics are far from static. They constantly shift, shaped by factors such as age, exercise, diet and where we live. Family members – including the furry variety – host similar microbial communities.
Most of our body’s resident microbes lurk in the nooks and crannies of our intestines, where they help break down food and ‘train’ our immune system against nasty infections.
And we know a healthy gut microbiome generally comprises diverse populations of microbes, with more ‘good’ bugs than ‘bad’, UNSW Professor of Medicine and consultant gastroenterologist Emad El-Omar says.
“Your gut faces many challenges and insults from the environment, such as food, toxins and drugs, so you want to have the skill mix within your gut to be able to deal with them all.”
It’s not just the blend of bugs living in our gut that matters. What they’re doing in there is just as crucial to our health.
Take the bacterium Escherichia coli. Most strains are harmless and dwell in our gut without any issues. But if pathogenic E. coli take hold, they churn out toxic metabolites that can cause diarrhoea, vomiting and kidney failure.
Yes – kidney failure. That’s because what happens in the gut does not always stay in the gut.
“Metabolites are the microbiome’s ‘currency of communication’”, El-Omar says.
When shuttled through epithelial cells lining the intestine and into the intestinal wall, metabolites can directly interact with the host’s enteric nervous system, consisting of around 100 million neurons, as well as the immune system. Approximately two-thirds of the body’s immune cells exist in the digestive system.
The intestinal wall is also rich in blood vessels, which whisk those metabolites to tissues around the body where they can stimulate cells into behaving in beneficial – and not-so-beneficial – ways.
“Some metabolites are vasopressors; they can tell the smooth muscle in your arteries to constrict, and that can increase blood pressure,” El-Omar says. “Some are short-chain fatty acids that have a direct impact on your metabolism, and others are neurotransmitters – your currency of communication with the nervous system.”
Defining ‘healthy’ to treat disease
Our gut microbiome’s reach extends around the entire body, so it shouldn’t come as a surprise that researchers in recent years have found ‘signature’ microbiomes for varied conditions such as dementia, obesity and some cancers.
And unlike our genes – which also play a role in disease development – our microbiome can be nudged away from a disease state to a healthier one.
“But first, we need to know what is normal,” El-Omar says. “If we can manipulate the microbiome to treat disease, you’ve got to know what to change it to.”
To this end, UNSW’s Microbiome Research Centre (MRC), which El-Omar founded and directs, is recruiting participants for the Healthy Optimal Australian Microbiome or HOAM study.
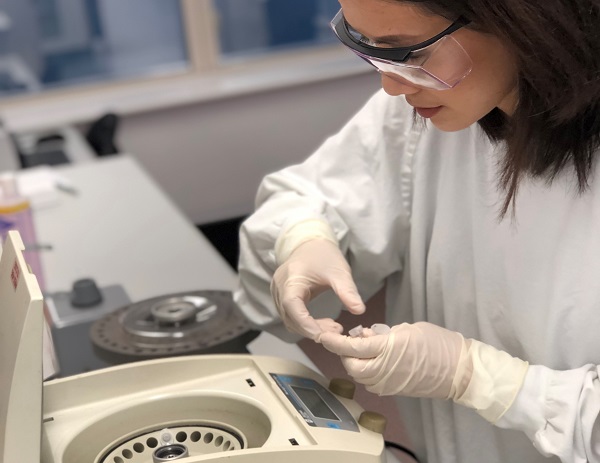
The project will take blood, stool, oral swab and urine samples from around 400 adults in tip-top condition, who eat a healthy and balanced diet, get plenty of exercise and avoid harmful behaviours such as smoking.
It will examine types of microbial species, decode the genes they switch on and sniff out metabolites they produce – taxonomic, transcriptomic and metabolomic analyses respectively.
Isabelle Ibrahim, registered nurse and HOAM study clinical manager, says the goal is to establish what an ‘optimal’ microbiome is using a “very high quality, very well rounded, holistic multi-omic” analysis.
“It’s a quick, cross-sectional snapshot, but it will be highly sophisticated,” she says.
“There’s a whole battery of metadata on top of the samples. A huge focus of the HOAM study is diet and eating habits. We’re also collaborating with researchers from other disciplines and have an organisational psychologist who’s developed a highly sophisticated cognitive assessment activity, so that will give us some really good data on the gut-brain link as well.”
Also included in the HOAM study will be an overweight or obese comparison group, as well as what El-Omar thinks will be the fascinating cohort: men and women aged 95 years or more with few or no cognitive deficits.
“These are the people who have survived all that the environment can throw at them, so they’re obviously made of the right stuff,” he says.
Ibrahim adds: “We’ll see who’s really flourishing the most out of all those groups – who’s not just survived but is living a good life – so we can capture the healthy optimal phenotype along the whole age span.”
Next up: clinical trials
Once HOAM establishes a healthy Australian microbiome benchmark, the MRC’s next step is to start clinical trials and restore disease-causing microbiomes to their optimal state.
This could be through diet or exercise, or therapies like targeted faecal microbiome transplants.
Instead of transplanting whole faecal donations between people, future treatments may provide refined ‘crapsules’ containing only the components needed to nurse a patient’s microbiome back to health.
Next-generation probiotics could also be on the table. Unlike the non-specific and often useless probiotics found on supermarket shelves today, these new biotherapeutics will contain organisms that treat specific conditions and be backed by clinical evidence.
While it may be years before the study reaches clinical trials, El-Omar says the pay-offs will potentially be huge.
“It’s worth the investment and all the hard work to recruit optimal people so you can have that template. It will allow patients to very rapidly generate an effective treatment action plan which – crucially – is backed by clinical evidence.”
By Bel Smith
Updated 2 months ago