A virtual pharmacy trial to reduce real-world medication errors in rural and remote areas
Hospital patients needing life-saving treatment can end up hospitalised for longer – or worse – because of a blunder with their medication.
It could be as simple as confusing two drugs with similar names or accidentally administering a double dose, but medication errors in hospital happen more often than you might expect. A 2016 review found that the rate of errors in prescribing medication in large teaching hospitals in Australia was on average, one prescribing error for each patient.
Hospitals in the bush are no exception. And with fewer resources, overstretched staff and geographical isolation, rural hospitals don’t have ready access to the suite of services their city counterparts do. But two years ago, Dr Shannon Nott, Rural Health Director of Medical Services for the Western NSW Local Health District, saw a prime opportunity to support his jurisdiction’s hospitals and reduce medication errors: set up a virtual hospital pharmacy.
Hospital pharmacists, as their name suggests, work in a hospital and have more of a clinical slant than retail pharmacists do. As well as preparing and dispensing medicines, hospital pharmacists work alongside clinicians to review patient medication charts, ensure medicines are appropriately prescribed and delivered, monitor patients for side effects, educate hospital staff and patients about therapeutics and provide a medication management plan to discharged patients.
But like most health professionals, hospital pharmacists are generally based in large hospitals in major cities. According to 2018 Australian Health Workforce Data, of the 5784 hospital pharmacists in Australia, 920 worked in regional areas, and only 54 of those areas were classified as remote or very remote.
“We don’t have access to hospital pharmacists in any of the small communities across rural NSW. And that would be consistent across most of Australia,” Nott says.
And this void poses a problem. Studies overseas and around Australia routinely show that when a pharmacist is involved with hospital patient care early in their stay, medication errors drop dramatically.
So Nott decided to deliver hospital pharmacy services to hospitals without an on-site pharmacy. In 2019, he received a Translational Research Grant from NSW Health to introduce a virtual pharmacy to eight rural hospitals in the Western NSW and Far West Local Health Districts – an area that, at more than 500,000km2, is about the size of Sweden.
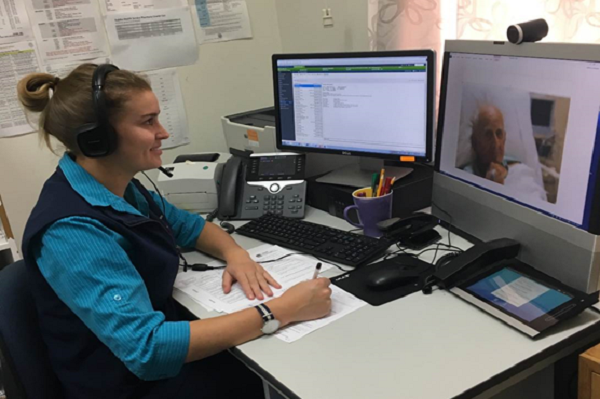
A roster of hospital pharmacists will be on hand to provide support for participating hospitals via advanced telehealth infrastructure. Remotely controlled by the pharmacist, a wireless trolley can trundle around wards. A high-definition camera and screen enables a virtual face-to-face service between the pharmacist and patient, their family and their clinicians. Compact devices, such as tablets, will also be used to communicate and provide medication reviews.
Seeing the patients and their medications provides a wealth of information to the pharmacist that a phone call can’t deliver, Nott says.
“A lot of patients don’t know what medications they’re on, so the pharmacists will be able to identify tablets based on their look. They’ll also work with general practices and community pharmacies to ensure that we’ve got the best possible medication histories for patients as well.”
He is currently recruiting his team and the first hospital will receive virtual pharmacy services in April. Rollout to the remaining seven sites will be staggered in one month intervals thereafter.
“But if we have additional capacity, and if the study and the results are going well, we may expand the service to other sites – just not include them as part of the research project,” Nott says.
After two years, Nott and his team will collect data about medication error rates and conduct interviews with patients, their family, pharmacists and hospital staff to get their thoughts on the trial. Meanwhile, the pharmacy service will remain operational in participating hospitals.
“Once the research component is closed out, we can make recommendations to the District and NSW Ministry of Health, and hopefully create a plan going forward to be able to sustain it for the long term,” Nott says.
A virtual pharmacy has applicability and translatability beyond the communities involved in the project, he adds, and if found to be a worthwhile venture, can be scaled up and expanded into other parts of the state or country.
“It’s exciting times, and once we get the pharmacy service up and running, I’m optimistic that it will be an effective way of assisting in medication management and minimisation of medication-related harm across our region.”
By Bel Smith
Updated 3 months ago