Tiny models promise large returns
“Using organoids … is relatively new and this is a service that has never been available before,” says Dr Anai Gonzalez Cordero. “Our hope is that it will speed up the development of safe and effective treatments for millions of children affected by genetic and acquired disorders.”
A pioneering facility producing models of human organs at Children’s Medical Research Institute (CMRI) is at the heart of treating a range of devastating diseases.
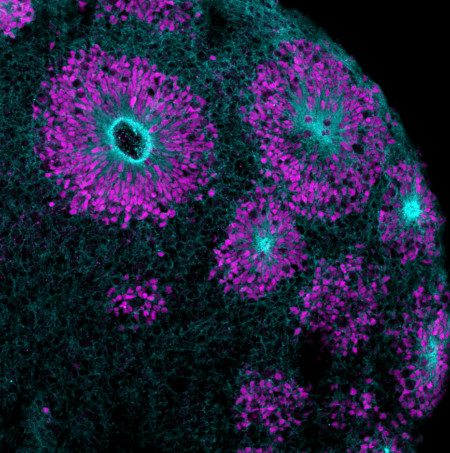
Until now, many genetic and acquired conditions have been incurable, but 3D mini organs derived from stem cells (known as organoids) promise exciting breakthroughs.
The Stem Cell and Organoid Service Facility, funded by Luminesce Alliance, is the only facility of its kind in Australia. Its expert team, led by Dr Anai Gonzalez Cordero, has perfected the culturing of organoids from induced pluripotent stem cells (iPSCs) which, in turn, are generated from a patient’s blood or skin. The organoids are often referred to as “mini organs” because they are so morphologically similar to actual organs, which has contributed to the rapid growth of this unique service.
In this brave new world of precision medicine, organoids are being used by clinicians and researchers to better understand disease progression, conduct analyses and test targeted treatments for diseases of the eye, brain, ear, kidney and heart.
“The beauty of stem cells is that they contain the same genetic condition as the patient, and we can use them to generate almost any organ we need to study,” Gonzalez Cordero says.
The Alliance – established with the support of an initial $20 million NSW Government grant – brings together the Children’s Cancer Institute (CCI), Children’s Medical Research Institute (CMRI), Randwick and Westmead campuses of the Sydney Children’s Hospitals Network (SCHN), and the University of New South Wales and University of Sydney as one of Australia’s largest paediatric research entities, heralding exciting new opportunities for further international collaboration.

Sharing technology and expertise
While her own research focuses on inherited retinal degeneration that causes blindness, Gonzalez Cordero is sharing her organoid expertise to support a variety of studies throughout NSW and across Australia.
“Using organoids in this way is relatively new and this is a service that has never been available before,” she says. “Our hope is that it will speed up the development of safe and effective treatments for millions of children affected by genetic and acquired disorders.”
It may even fast-track medical intervention. “The very early access to tissue gives us the opportunity to determine if bio-markers or features of the disease are present early in a child’s life,” Gonzalez Cordero says. “That may enable us to intervene and introduce treatment much earlier than ever before.”
Mini ‘brain in a dish’
One inspiring example of the utility of the Stem Cell and Organoid Service Facility is its role in the work of Associate Professor Wendy Gold, head of the Molecular Neurobiology Research Group at Kids Research (SCHN). She is studying brain disorders in children at the molecular level, including rare terminal conditions that cause severe seizures.
To develop and validate potential treatments, Gold is collaborating with Associate Professor Leszek Lisowski, head of the Translation Vectorology Unit at CMRI, whose expertise is in developing the advanced therapeutics and new mechanisms (vectors) for delivering gene therapies to the patients.
“To test therapies, we use organoids that Anai has created – mini brains in a dish with the very disease the patient has,” says Lisowski. “Those are very effective patient-specific and disease-specific models. We can test both the delivery vector and the therapeutic cargo in the organoid.”
With two promising treatments in advanced development, the strength of this collaboration is already evident.
“The facility allows us to do this kind of translational research, to find solutions together,” Gonzalez Cordero says. “That’s the power of the Luminesce Alliance. It has brought us into partnership – the clinical side, human stem cell biology, omics, computational biology, gene therapy and medicinal chemistry – to develop therapies that are now being trialled.”
With the ability to generate thousands of organoids at a time, Gonzalez Cordero’s team is now in high demand. And for good reason.
“The work we are doing using organoids is providing hope to patients who might otherwise perish,” Lisowski says. “It’s giving them a chance.”
Discover more about how the alliance was formed with the support of NSW Health here.
View a short video about Functional Genomics – Stem Cells.
Updated 3 years ago