Medicine and engineering join forces to save lives
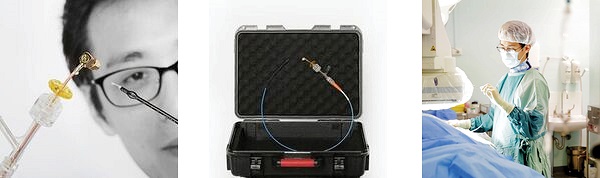
A marriage of engineering and medicine in Western Sydney has borne fruit with a breakthrough device that looks set to save lives – a microwave-emitting catheter to control high blood pressure.
The device, known as the “Mu Catheter”, uses microwaves to perform “renal denervation” – a procedure to treat drug-resistant high blood pressure.
The device was co-invented by cardiologist Dr Pierre Qian and biomedical engineer Tony Barry, both PhD students with the University of Sydney and employed at Westmead Hospital, which has a long history of important collaborations between engineers and doctors.
The invention was awarded $1.39 million by the NSW Medical Devices Fund in 2017 to support commercial development.
As a result, the pair are about halfway through the lengthy process of refining prototypes, having tested the device in-vivo and preparing for a six-month trial shortly. All things going to plan, the first human patient trial should begin soon after that.
So far, the developments are promising.
Controlling blood pressure
“It’s working,” says Barry. “It’s doing a job that is as good or better than the competition, and at the same time it’s a whole lot easier to use with a whole lot fewer headaches.”
The Mu Catheter began life as an idea Qian had as a resident medical officer, in his second year of training in cardiology.
At that time, Qian and his colleagues were interested in looking at new ways of ablating heart muscle – a medical procedure that inactivates the tissue that triggers abnormal heart rhythms.
One of Qian’s projects was looking at ways to design a micro catheter that could be used for ablations in the atrium – or upper chamber of the heart.
“Tony and the department had done a lot of work on microwave ablations over the past 15 years or so,” says Qian. “We went through a lot of different antenna designs.”
In the process they discovered that if a microwave catheter didn’t have any contact with the heart muscle it would spare the surface tissue – which for cardiac ablation is not such a good thing.
“You want to make a transmural lesion,” says Qian. “That is, you want to make a lesion that’s full thickness, and having a region of surface unaffected for a millimetre or more is detrimental.”
But what was bad for the heart, was good when performing the procedure on the renal, or kidney, nerves which surround the artery, relaying information between the kidneys and cardiovascular and nervous systems.
These nerves are hyperactive in many people with difficult-to-control blood pressure, but they can be deactivated using heat.
“We realised that this could be very good for renal denervation,” says Qian.
Avoiding artery damage
“The aim of that is the same as with the heart, to make a certain central lesion, except in the case of renal denervation we do want to spare the tissues adjacent to the blood flow because those are arterial tissues.
“And so we want to preserve the artery while ablating around it,” he says.
But the confined space of the renal artery dictated a change of design from the traditional catheter – which led to the unique Mu Catheter’s shape.
“The current design became more obvious as we tried to investigate ways of designing a microwave catheter that could fit in the renal artery,” says Qian.
“Many features of current microwave designs add bulk to the catheters, so we ended up removing those features, and testing to see how a catheter like that would work.
“And it turned out that it was actually better, to our surprise.”
Key funding to bring device to market
The unique feature of the Mu Catheter is the small microwave radiator, insulated from the blood pool and surrounded by an expandable sheath, which centres the radiator in the renal artery but still allows blood to flow through the artery while the procedure is underway.
“It radiates microwaves into the tissues surrounding the renal artery to provide a deep and circumferential ablation to consistently reach most of the renal nerves,” says Qian. But at the same time, it avoids injury to the renal artery itself which is cooled and protected by blood flow.
Despite its promise, the device may have stayed in the lab had it not been for the NSW Medical Devices Fund.
Pierre Qian says, “We applied for a lot of grants, and we got initial seed capital of $23,500 from the University of Sydney and the Western Sydney Local Health District.”
“It was due to that seed capital that we were able to get a whole lot of preclinical data that was very compelling”.
After pitching to seven or eight venture capital funds, they approached the NSW Medical Devices Fund.
“And we ended up getting that, which was fantastic. On the back of that we are now designing the catheter as a proper medical device rather than a prototype. We’re hoping to have a final – or very close to final – clinical device that’s functional for a trial leading to first-in-man studies, we’re hoping mid-year”.
Tony Barry puts it more bluntly.
I don’t know how to say this nicely, so I’ll say it straight. We’re poverty stricken researchers. We go around begging for stuff. And because we usually haven’t got much, the $1.39 million for the Mu Catheter represents the biggest chunk of funding we’ve seen in a long time.
“So I can’t say enough about how good the NSW Medical Devices Fund has been for us.”
By Bill Condie
Updated 5 years ago