How tiny lab-grown organoids are providing human-specific research results
Mini organ-like complexes called organoids, are part of a growing range of non-animal technologies helping to reduce and replace animal testing in research.
In 2009, Dutch molecular geneticist Professor Hans Clevers grew a miniature organ called an organoid in the lab. The tiny intestine replica was a significant breakthrough that showed human stem cells could self-organise and mimic the architecture and function of real organs. Fast-forward fifteen years and 3D organoids are now being used to test new treatments for diseases of the lung, eye, brain, ear, kidney and heart.
To further advance development and use of organoids and other non-animal technologies the Office for Health and Medical Research formed the Non-Animal Technologies Network in 2024. Dr Shafagh Waters is a founding member of this Network and a Scientia senior lecturer at UNSW, Sydney, which is a key partner in the Network. Waters is an expert in stem cell and organoid medicine and an honorary senior scientist at Sydney Children’s Hospitals Network. She has developed an Australian national biobank of airway and gut organoids and leads a National Health and Medical Research Council funded research program on adult-stem-cell biology for Cystic Fibrosis. The Office spoke to Dr Waters to find out more about organoids and how she is using them in her research.

How do organoids work?
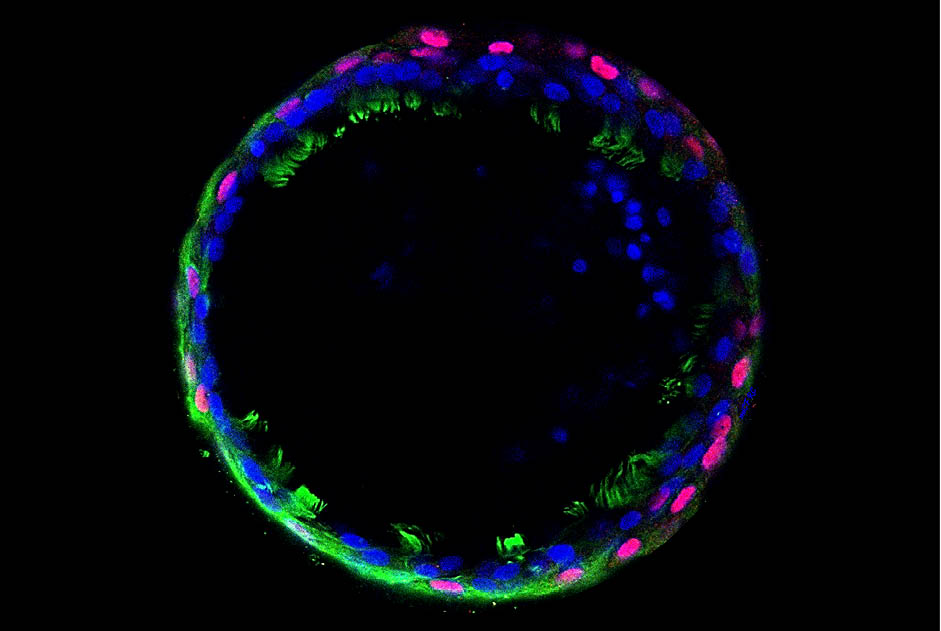
“Organoids mimic the structure and function of real organs, but on a much smaller scale. They are grown from stem cells in a lab and, once they develop, they start to behave like the organ they represent. For example, lung organoids have cells that can absorb oxygen and produce mucus, just like real lungs do. Because they have many of the same cells and functions as the actual organ, researchers can use them to study how diseases affect these tissues or test a new drug to see if it helps improve the organoid lung function.”
How are organoids made?
“Organoids are made by brushing the tissue of interest or taking a small biopsy to collect the stem cells, which have the ability to grow into different types of cells. With lung organoids for example, we guide the stem cells to develop into lung-like structures by placing them in a special gel that supports them. We also feed them nutrients which give the right “instructions” so the cells know what to become. Over time, the stem cells start to organise themselves and form 3D structures that resemble tiny versions of the organ or tissue we’re interested in.”
How are you using organoids as ‘avatars’ in your research?
“We’ve developed lung and gut ‘avatars’ which are miniature versions of these organs using patient-derived stem cells. They closely mimic the structure and function of the mucosal lining and allow us to test medications and personalise therapies to meet their specific needs. In the future, I envision our work leading to a companion diagnostic test. This would use an avatar organoid from a patient with Cystic Fibrosis to predict how well they will respond to a particular treatment and it would guide doctors in choosing the most effective therapy.”
How is the Network supporting your work?
“The Office for Health and Medical Research has been key in fostering collaborations and opportunities to advance non-animal technologies. Funding through the Network is allowing us to really advance our research on complex-organoid technologies and link these with the infrastructure being set up in NSW for scaling up production. This also includes high-throughput testing using organoids, which is a method that quickly tests thousands of drug compounds at once using automated systems, helping scientists find effective treatments faster.”
What kinds of mini organs can now be made with organoids?
“Using organoids, we can now create many types of mini-organs. These include:
– Lungs: to study respiratory diseases like Cystic Fibrosis
– Intestines: used to research gut health, cancer, and infections
– Brain: for studying neurological disorders such as Alzheimer’s or autism
– Kidneys: to explore kidney disease and test treatments
– Liver: for drug testing and liver disease research
– Pancreas: for studying diabetes and pancreatic disorders
– Stomach: to investigate digestion and diseases like gastric cancer.”
Patient-derived organoids allow researchers to closely mimic human biology, improving the ability to test therapies and understand complex conditions. They provide more human-specific results that are more accurate than animal testing and helping the development of more personalised treatments.”
Read more about the Network
Updated 5 months ago