Discovery of immune cells in the brain creates new possibilities for schizophrenia treatment
In Australia, schizophrenia affects around 2.4 per 1,000 people, and despite decades of research, there is no cure. Drug therapies treat some symptoms, such as psychosis, but not others – nor do they address the disease’s underlying drivers.
This may soon change, thanks to work led by Neuroscience Research Australia and University of NSW’s Professor Cyndi Shannon Weickert. The NSW Chair of Schizophrenia Research and her team have discovered a new player in the disease’s brain pathology: immune cells. Armed with this knowledge, she is collaborating with immunologists to swiftly test more effective treatments.
“To discover immune cells in the brain was unexpected, and now the whole field is having this awakening phenomenon,” Shannon Weickert says.
But the breakthrough arose by accident. At the time, Shannon Weickert wasn’t poking around schizophrenia brain tissue looking for immune cells. Instead, she was pursuing a change in a gene regulatory protein known to impair brain development.
“A graduate student came to me and said, ‘I’ve figured out what’s different in the schizophrenia brain. It’s inflammation,’” Shannon Weickert says. “I said, ‘This can’t be right. There’s no inflammation in the brain. Let’s analyse the data again.’”
Despite reanalysis, those tell-tale signs of inflammation – the presence of molecules called cytokines – stubbornly persisted. And Shannon Weickert realised her team was onto something big.
White blood cells in white and grey matter
Doctors don’t know for certain what causes schizophrenia, but the notion that the immune system has a hand in its development has been kicking around for some time. Large genetic studies support the idea. Yet for most of the 20th century, the brain was deemed “immune-privileged”, with its primary – and only – line of immune defence comprising resident cells called microglia.
Immune cells coursing through the bloodstream were denied entry to the brain by the blood-brain barrier, a layer of tightly packed endothelial cells lining brain capillaries – or so it was once thought.
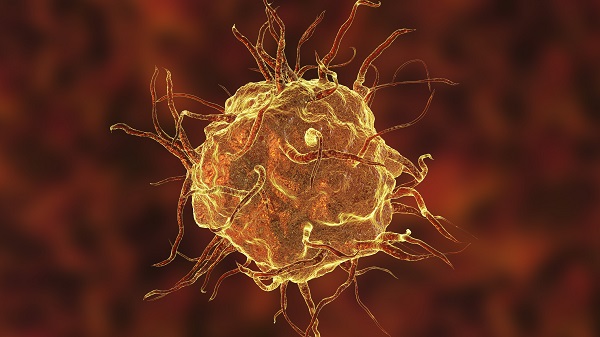
Shannon Weickert and her crew showed that the inflammatory cytokine-secreting culprits in schizophrenia brains included white blood cells called macrophages, which were snared and allowed passage by the very cells forming the blood-brain barrier.
“We saw glial cells in the brain become inflamed and send distress signals to endothelial cells,” Shannon Weickert says. “We think this causes the endothelial cells to become ‘stickier’ and capture more of the macrophages in the blood as they cruise by, so they’re more likely to make it into the brain and cause inflammation.”
While healthy brains contained low levels of cytokines, brains with schizophrenia had dramatically higher levels. Indeed, macrophages were found close by neurons in some of the people who had schizophrenia accompanied by high brain inflammation.
The team unveiled their macrophage discovery in Molecular Psychiatry in 2018, where they reported on the prefrontal cortex, the part of the brain located just behind the forehead. It’s implicated in complex cognition, decision-making and social behaviour – attributes affected early in the progression of schizophrenia.
They have since found high levels of macrophages in other areas of schizophrenia brains. These include the midbrain – where dopamine neurons reside, and which is implicated in the disease’s pathology – and the subependymal zone, which churns out new brain cells. Shannon Weickert hopes to publish this work soon.
Inflammation: a therapeutic target
So how do brain macrophages influence schizophrenia development? Shannon Weickert suspects brain trauma – from, for instance, drug abuse or stress – may kick off an inflammation cascade that leads to schizophrenia in those with a genetic predisposition to the disorder.
Normal controlled inflammation in the body is beneficial: it attracts immune cells, which conduct repairs and clean up cell debris. But instead of the immune system dialling down inflammation with healing, it can sometimes be ramped up.
“And in the brain, immune cells can make a bad situation worse by secreting too many pro-inflammatory cytokines for too long, damaging more neurons, creating more inflammation, and so on,” Shannon Weickert says.
A potential way to break this cycle is to dampen a master regulator of the immune system. Calmer blood macrophages may be less likely to overreact and generate inflammation if they end up in the brain. Another is to encourage brain macrophages to become anti-inflammatory so they aid repair – not hinder it.
To expedite the hunt for therapeutics, Shannon Weickert partnered with immunologists to trial medications, developed for other diseases that act on the immune system and have already been shown to be safe in clinical trials. One – or some – of these existing drugs may also help an inflamed brain to settle down.
Her recent work, Shannon Weickert acknowledges, would not have been possible without a $4 million grant awarded by NSW Health in 2017.
“Having this kind of support allows you to turn on a dime and take advantage of new technology as it appears. With next-generation sequencing, for instance, we were the first to identify the increase in macrophage pro-inflammatory cytokines.”
It’s not just professional interest that keeps Shannon Weickert motivated – it’s personal too. Her twin brother, Scott, was diagnosed with schizophrenia as a teenager, and he died in 2008.
“Few researchers feel the pain of those that are suffering from the illness as keenly as I do because I lost my brother to the disease,” Shannon Weickert says.
“We can’t give up, but we’re getting much closer to a cure.”
By Bel Smith
Updated 2 years ago