Blood pressure drugs may bring clarity to new COVID-19 treatment
Common blood pressure medication is at the centre of a new COVID-19 treatment clinical trial led by the George Institute for Global Health.
The CLARITY study, which received $1.4 million from the Australian Government’s Medical Research Future Fund in June, is recruiting patients in Australia now, and, will soon do the same in India.
And while blood pressure drugs may not seem particularly relevant to an infectious respiratory disease at first glance, they do have a biological connection, says UNSW Medicine’s Associate Professor Meg Jardine, who is the CLARITY trial leader and Program Head of Innovation & Kidney Research at the George Institute.
“We see generally that people with chronic health conditions, such as high blood pressure, chronic kidney disease, diabetes, cardiovascular disease and obesity, are also those who are more vulnerable if they contract COVID-19 infection.”
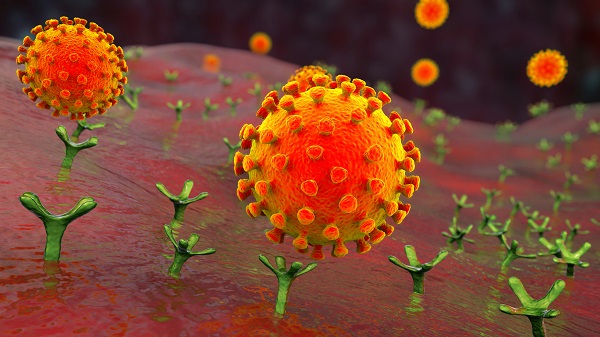
The best recognised site of infection from the SARS-CoV-2 virus – which causes COVID-19 disease – is in the lungs. The virus latches onto a protein called angiotensin-converting enzyme 2 (or ACE2), which is found on the surface of some lung cells, and tricks the cell into internalising or ‘swallowing’ it. Once inside, the virus hijacks the cell’s machinery and replicates.
The virus also downregulates and suppresses ACE2’s anti-inflammatory effects, Jardine says. “And that may tip the local lung environment towards inflammation and fibrosis, and might be why the virus has such a devastating effect on lung tissue.”
Eventually, thousands of copies of the virus burst out of their host cell and slip into others – and they’re not limited to the respiratory system. ACE2 molecules are found in cells throughout the body. It’s thought this is why SARS-CoV-2 can inflict damage on tissues found in blood vessels, the kidneys, gut, heart and even the nervous system – all of which express ACE2.
But SARS-CoV-2’s route inside human cells may have an Achilles heel. To successfully invade a cell, the virus requires another membrane protein: an angiotensin receptor.
Using a group of blood pressure drugs that block these receptors – appropriately called angiotensin receptor blockers or ARBs – the CLARITY study hopes to thwart SARS-CoV-2’s potentially deadly spread through the body.
Old drug, new tricks?
ARBs are cheap, readily available and have been prescribed for more than 30 years. They help reduce blood pressure by stopping angiotensin, a hormone that instructs blood vessels to constrict from binding to its receptor.
And evidence from animal trials suggests ARBs may be a promising treatment for COVID-19. For instance, a mouse study published in Nature Medicine found that an ARB called losartan protected lungs against damage inflicted by the coronavirus SARS-CoV-1, which spread around the world in 2003.
But it isn’t known yet whether ARBs can afford humans the same protection. To find out, the CLARITY trial has been approved to run in multiple locations across New South Wales, Victoria and India.
Jardine and her colleagues – including the head of the George Institute’s India office and fellow nephrologist Dr Vivekanand Jha – started recruitment in Australia and hope to begin recruiting in India in July.
Patients will be invited to participate if they are admitted to hospital with COVID-19 or are from a high-risk group and being monitored at home. In Australia, consent to participate can be verbal to minimise in-person contact.
Half of the participants will receive an ARB, and the study will mostly focus on collecting information around effectiveness and common side effects, so will be partially integrated into routine clinical care, Jardine says.
Given the current lack of COVID-19 treatments or vaccines, interventions that can alleviate the disease’s severity in any way are desperately needed. Repurposing existing medications is an attractive strategy as it eliminates development time and costs, and, once verified through randomised trials, the medications can be rapidly included in standard clinical care.
“Unlike trials for new agents, we know a lot about ARBs. What we don’t know is whether they may alter the course of COVID-19 disease, and that’s the question CLARITY is designed to answer,” Jardine says.
And when medical research is embedded in the health system, everyone benefits, she adds. “Patients will often be interested in participating in multiple research studies and our consumer representatives have backed this collaborative approach. You address clinical questions more efficiently, which means incorporating more proven treatments into clinical practice more quickly – and really, that’s the goal.
“The world can’t wait to answer these questions one at a time.”
By Bel Smith
Updated 5 years ago