Detecting rogue cells and DNA differences to improve arthritis monitoring and treatment
A new research project will investigate the underlying drivers of arthritis and why many people experience complications and less effective relief from treatments.
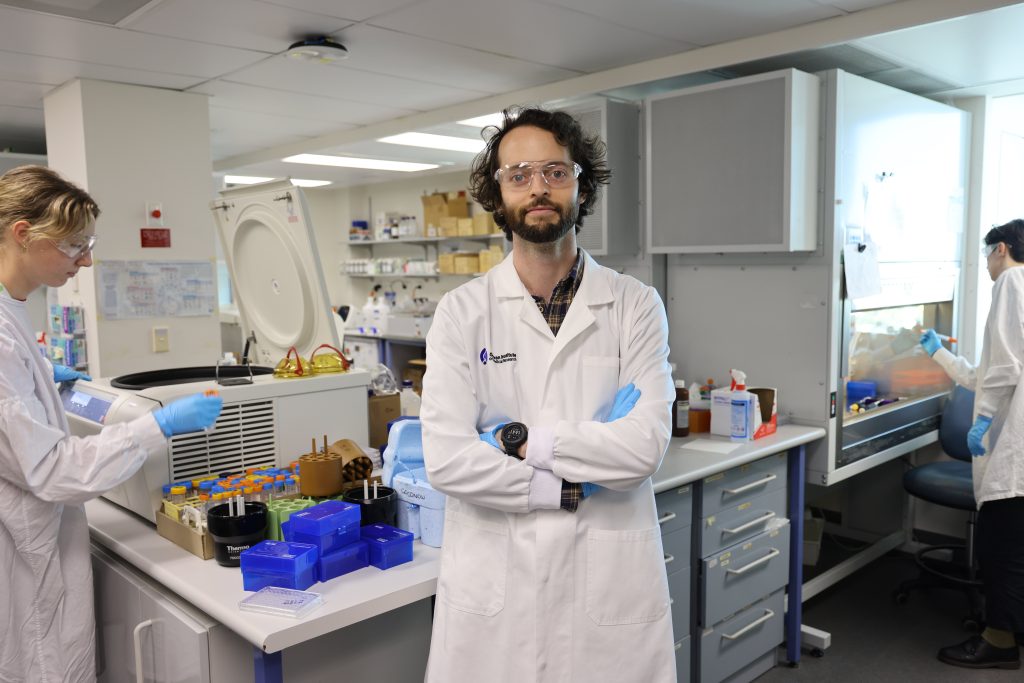
What role do rogue cells within the body play in triggering and worsening arthritis? Dr Etienne Masle-Farquhar, Research Officer at the Garvan Institute of Medical Research, is on a mission to find out. As Chief Investigator of ‘Blood and Bone: a multiomic study of arthritic joints’, he and his multidisciplinary team of collaborators aim to improve evidence-based monitoring and treatment of arthritis, the leading cause of chronic pain.
“We hope to identify the specific cellular and molecular mechanisms that drive development and progression of arthritic diseases, to establish evidence-based guidance to aid clinicians in selecting appropriate treatments and predicting their efficacy,” Masle-Farquhar explains.
NSW Health Early-Mid Career funding support
Funding support of $500,000 over three years has been provided for the project by the Office for Health and Medical Research, via an Early Mid-Career Grant. “This grant is enabling us to sustainably grow our clinical network, our high-quality biobanking and our research,” says Masle-Farquhar. “It is supporting talented, passionate staff required to perform cutting-edge experiments, to make scientific and clinical impacts, and pave the way for additional grant applications that will secure our arthritis biobanking and research program, as a long-term hub within NSW.”
A disease with many faces
Rheumatoid arthritis is the most prevalent autoimmune disease, affecting over 500,000 Australians. Osteoarthritis is the most common form of arthritis, affecting over two million Australians and 500 million people worldwide. “Arthritis disproportionately affects the elderly, individuals in rural areas and Aboriginal people,” says Masle-Farquhar. “Certain forms of arthritis can also seriously affect groups such as women, children and young men in their 20s to 30s.”
In addition to joint pain, arthritis can cause stiffness and swelling, and may decrease range of motion of joints, muscles and tendons. Arthritic diseases impact relationships, mental wellbeing and quality of life of patients and their families. “They are also associated with increased risk of systemic complications, including heart disease, lung disease, infections, osteoporosis and accelerated cognitive decline,” Masle-Farquhar explains.
Rogue cells and gene mutations
Rogue immune cells don’t work like healthy immune cells and they have been linked to the development of diseases. “Our research will explore whether rogue cells, and potentially different types of rogue cells, play critical roles in initiating or accelerating arthritis development, progression, resistance to treatments and onset of systemic complications,” says Masle-Farquhar.
“One aim of this project is to investigate whether acquired mutations contribute to arthritis and its disease outcomes. ‘Acquired mutations’ are modifications to DNA that are not inherited from parents, but are acquired within only a subset of cells. “We aim to explore whether random acquisition of mutations may help to explain unpredictable onset of disease and variable treatment outcomes,” Masle-Farquhar says.
Developing an extensive biobank of samples
To inform their research, the team is establishing a unique biobank that stores clinical data and diverse samples from people who have arthritis or other diseases. “These precious biospecimens maximise the number of scientific and clinical questions that we can address,” says Masle-Farquhar. The samples include blood, saliva, synovial tissue (which lines the cavities between joints and is degraded or attacked in most forms of arthritis) and synovial fluid (which surrounds the joint and can accumulate excessively during flares and inflammation). Bone marrow (where immune cells develop) and bone (which contains many cells contributing to arthritis and osteoporosis), will also be collected.
The biobanked samples are donated by patients and their treating physicians within St Vincent’s Private Clinic, St Vincent’s Public Hospital, St Vincent’s Private Hospital, Westmead Hospital, St George Private Hospital and East Sydney Private Hospital, and they are securely stored at the Garvan Institute of Medical Research.
DNA detective work
This project will use “multiomics”. This approach combines the data from the study of DNA, RNA, epigenetic changes (chemical modifications on DNA molecules) and proteins to determine which genes are being switched on and off and what instructions are being given to cells.
“Our research is using advanced technologies such as single-cell genome sequencing (studying genetic information of individual cells),” says Masle-Farquhar. “These approaches give us unprecedented power to identify and study cells that have gone rogue.”
The data obtained may help identify a specific cell population or molecule that causes arthritis, or acts as a biomarker for the disease. “We hope it will help clinicians then identify patients likely to respond (or not respond) to specific treatments, or develop (or not develop) flare-ups, chronic pain or specific conditions linked to arthritis, such as lung or heart disease,” says Masle-Farquhar “In the longer term, this will help to us to improve arthritis disease monitoring and diagnosis as well as most the appropriate targeted therapies to improve patient outcomes and lives.”
Updated 3 weeks ago